OBJECTIVES:
•What is amniotic fluid?
• Physical characteristic and Volume
• Chemical Composition
• Amniotic fluid production
• Amniotic fluid circulation
• Functions
• Amniocentesis
• Amniotic fluid index
• Abnormalities
•Polyhydramnious
• oligohydramnious
•Amniotic fluid: or liquor amnii is a clear, slightly yellowish liquid that surrounds the unborn baby (fetus) during pregnancy.
• It is the nourishing and protecting liquid
• It is found within the amniotic sac contained in the mother's womb.
Physical characteristics
• It is clear pale yellow fluid.
• pH of is around 7.2.
• Specific gravity of 1.0069 – 1.008.
volume:
volume depends on gestation
As a very rough guide, total volumes are about:
•30 ml at ten weeks,
•300 ml at twenty weeks,
•600 ml at 30 weeks and
•about a litre at thirty-eight weeks.
•Beyond this point, the volume gradually falls
•It will be about 800 ml at forty weeks and lower still if the pregnancy continues to forty-one or forty two weeks.
Chemical composition:
•The composition of the amniotic fluid changes with gestation in early pregnancy it is similar to maternal and fetal serum.
• 98-99% of the amniotic fluid is water.
•A large number of dissolved substances such as: creatinine, urea, bile pigments , renin, glucose ,fructose, proteins (albumin and globulin) , lipids, hormones (estrogen and progesterone ), enzymes , minerals (Na+ ,K+ Cl- )
• un-dissolved substances like fetal epithelial cells .
• during the second half of gestation its osmolarity decreases and is close to dilute fetal urine with added phospholipids and other substances from fetal lung and other metabolites .
Amniotic fluid production:
•At very early stages the amniotic fluid is secreted by the amniotic cells .
- Later most of it is derived from the maternal tissue fluid by diffusion, across the amniochorionic membrane and from the placenta.
- A little is contributed by fetal respiratory secretions through the skin which becomes less later in progressed pregnancy since the fetal skin becomes less permeable .
- By 11th week, fetus contributes to amniotic fluid by urinating into the amniotic cavity; in late pregnancy about half a liter of urine is added daily.
- After about 20 weeks, fetal urine makes up most of the fluid.
Amniotic Fluid: Circulation
•The water content of the amniotic fluid changes every three hours
•Large volume moves in both directions between the fetal & maternal circulations mainly through the placental membrane
•It is swallowed by the fetus, is absorbed by respiratory & GIT and enters fetal circulation. It then passes to maternal circulation through placental membrane. During final stages of pregnancy fetus swallows about 400ml of amniotic fluid per day
•Excess water in the fetal blood is excreted by the fetal kidneys and returned to the amniotic sac through the fetal urinary tract
Amniotic Fluid: Functions:
•Amniotic fluid is "inhaled" and "exhaled" by the fetus. It is essential that fluid be breathed into the lungs in order for them to develop normally.
•Swallowed amniotic fluid also creates urine and contributes to the formation of meconium .
•The fetus floats in the amniotic fluid. It allows fetus to move freely, aiding development of muscles and bones.
•Acts as a cushion to protect embryo from mechanical injuries.
•Permits normal fetal development.
•Acts as a barrier to infection ,(transferrin in the amniotic fluid binds iron needed by some bacteria and fungi ,fatty acids have a detergent effect on bacterial membranes and contains Ig and lysozomes that also help in fighting pathogens)
• Assists in regulation of fetal body temperature, protecting from heat loss
• Prevent adherence to the amnion
• Helps in dilatation of cervical canal at the time of birth
• Amniotic fluid is also a plentiful source of non-embryonic stem cells . These cells have demonstrated the ability to differentiate into a number of different cell-types, including brain, liver and bone
Amniocentesis:
•Amniocentesis is the removal of a small amount of amniotic fluid from the sac around the baby.
• This is usually performed at 16 weeks (2nd trimester) in pregnancy.
• A fine needle is inserted under ultrasound guidance through the mothers' abdomen into a pool of amniotic fluid.
Studies of the cells obtained from the amniotic fluid permit:
1- Chromosomal analysis of the cells which can be performed to investigate the following;
§Diagnosis of sex of the fetus
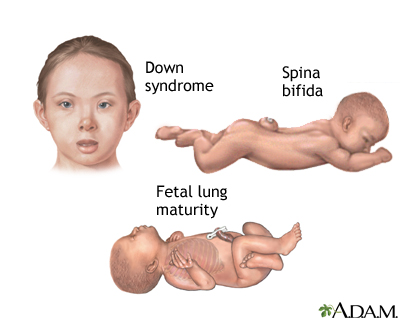
§Detection of chromosomal abnormalities e.g. trisomy 21(Down’s syndrome)
§DNA studies
2- The cells may be cultured and analyzed for enzymes, or for other materials that may indicate genetically transmitted diseases
§( Inherited disorders e.g Cystic Fibrosis).
3-To check for developmental problems e.g. Spina Bifida . Babies born with spina bifida have a backbone that did not close properly. Serious complications of spina bifida can include leg paralysis, bladder and kidney defects, brain swelling (hydrocephalus), and mental retardation.
4- Other studies can be done directly on the amniotic fluid including measurement of alpha-fetoprotein
–high levels of alpha-fetoproteins indicate the presence of a severe neural tube defect
–whereas low levels of alpha-fetoproteins may indicate chromosomal abnormalities .
Who is the proper candidate for an Amniocentesis investigation? 1-Those whom are suspected to have possible problems indicated by certain tests conducted previously ,(e.g If pregnancy is complicated by a condition such as Rh-incombatibility, the doctor can use amniocentesis to find out if the baby's lungs are developed enough to endure an early delivery).
2- Family history of genetic abnormalities (in this case would be advisable to seek genetic counseling before becoming pregnant)
What are the risks of amniocentesis?
Like any invasive procedure there are risks, which are:
•- Abortion: about 1 in 200 to 400 women aborted (higher risk if done in the first quarter)
•- Uterine infection: 1 in 1000
When are the results be obtained?
• It might take two weeks or shorter depending on the test required .Having it done in minimum time is important so that the decision can be made at the proper time depending on the outcome
•Examples of Other Tests performed on the amniotic fluid :
a)Measurements of the lecithine/sphingomyelin ratio ( as the lung matures the concentration of phospholipids especially lecithin increases since it is the major lung surfactant). This test is done to assess the maturation of the fetal lungs , a ratio 4/1 indicates mature lungs and a ratio less than 4/1 indicates immature lungs.
b) Measurements of bilirubin indicates the degree of fetal red blood cell destruction ,where abnormally high levels could indicate serious cases such as mother fetal blood incompatibility
Amniotic Fluid Index:
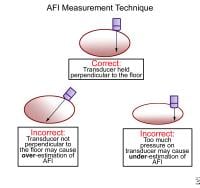
•Amniotic fluid index (AFI) is a rough estimate of the amount of amniotic fluid and is an index for the fetal well-being. It is a part of the biophysical profile .
•AFI is the score (expressed in cm) given to the amount of amniotic fluid seen on pregnant uterus and calculated by a ultrasonograph (aka ultrasound). To determine the AFI, doctors may use a four-quadrant technique , when the deepest, unobstructed, vertical length of each pocket of fluid is measured in each quadrant and then added up to the others , or the so called "Single Deepest Pocket" technique
•A normal AFI is about 12.
•But 8-18 is normal
•AFI < 5-6 = oligohydramnios (oligo, less; hydramnios, fluid)
•AFI > 18-22 = polyhydramnios
(poly, much or many)
ABNORMALITIES
Polyhydramnios:
Polyhydramnios means having too much amniotic fluid in the uterus (womb) more than 1500-2000 ml
Polyhydramnios signs and symptoms:
• Are a result of pressure being exerted within the uterus and on nearby organs, may cause:
• Shortness of breath or the inability to breathe, except when upright
• Swelling in the lower extremities, vulva and abdominal wall
• Decreased urine production
CAUSED BY:
• A birth defect that affects the baby's gastrointestinal tract or central nervous system
•Maternal diabetes
• Twin-twin transfusion — a possible complication of identical-twin pregnancies in which one twin receives too much blood and the other too little
•A lack of red blood cells in the baby (fetal anemia)
•Blood incompatibilities between mother and baby
•the placenta may have developed a tumour
§ there may be a problem with the arteries in the umbilical cord resulting in polyhydramnios.
Complications of polyhydroamnios
Polyhydramnios may increase the risk of:
• Premature birth
• Pregnancy-induced high blood pressure
• Urinary tract infections during pregnancy
• Premature rupture of membranes
• Excess fetal growth
• Placental abruption — when the placenta peels away from the inner wall of the uterus before delivery
• Umbilical cord prolapse — when the umbilical cord drops into the vagina ahead of the baby
• C-section delivery
• Stillbirth
•Heavy bleeding due to lack of uterine muscle tone after delivery
TREATMENT of polyhydroamnios:
•Drainage of excess amniotic fluid.
• Medication.
oral medication indomethacin to help reduce fetal urine production and amniotic fluid volume
Oligohydramnios:
A deficiency in the amount of amniotic fluid in the gestational sac during pregnancy less than 400ml.
AETIOLOGY:
FETAL
•PROM (50%)
•CHROMOSOMAL ANOMALIES
•CONGENITAL ANOMALIES
•IUGR
•IUFD
•POSTTERM PREGNANCY
MATERNAL
•PREECLAMPSIA
•APLA SYNDROME
•CHRONIC HT
PLACENTAL
•CHRONIC ABRUPTION
•TTTS
•CVS
DRUGS
•PG SYNTHETASE INHIBITORS
•ACE INHIBITORS
IDIOPATHIC
COMPLICATIONS:
FETAL
Abortion
Prematurity
IUFD
Deformities –CTEV,contractures,amputation
Potters syndrome- pulmonary hypoplasia
Malpresentations
Fetal distress
MSAF – MAS
Low APGAR
MATERNAL
Increased morbidity
Prolonged labour: uterine inertia
Increased operative intervention
(malformations, distress)
TREATMENT:
•ADEQUATE REST – decreases dehydration
•HYDRATION – Oral/IV Hypotonic fluids(2 Lit/d)
temperory increase
helpful during labour,prior
to ECV, USG
•SERIAL USG – Monitor growth,AFI,BPP
•INDUCTION OF LABOUR/ LSCS
Lung maturity attained
Lethal malformation
Fetal jeopardy
Sev IUGR
Severe oligo
AMNIOTIC FLUID EMBOLISM:
AFE is thought to occur when amniotic fluid , fetal cells, hair, or other debris enter the maternal circulation
Presentation:
there will be profound respiratory failure with:
deep cyanosis
• cardiovascular shock
• convulsions and
• profound coma
Causes:
•Ruptured membranes (a term used to define the rupture of the amniotic sac )
•Ruptured uterine or cervical veins
•A pressure gradient from uterus to vein
•A maternal age of 35 years or older,
• caesarean or
•placenta previa or abruption,
•eclampsia , and
•Time of event:
- During labor.
- During C/S.
- After normal vaginal delivery.
- During second trimester TOP.
• AFE syndrome has been reported to occur as late as 48 hours following delivery.
Risk factors of AFE:
•Advanced maternal age
•Multiparity
•Meconium
•Cervical laceration
•Intrauterine foetal death
•Very strong frequent or uterine tetanic contractions
•Sudden foetal expulsion (short labour)
Placenta accreta
•Polyhydramnios
•Uterine rupture
•Maternal history of allergy or atopy
•Chorioamnionitis
•Macrosomia
•Male fetal sex
•Oxytocin (controversial)
Nevertheless, these and other frequently cited risk factors are not consistently observed and at the present time
Experts agree that this condition is not preventable
•